This Study Moves Us Closer To Understanding Epilepsy While Personalizing Treatment Options

Approximately 2.9 million U.S. adults ages 18 and older reported having active epilepsy during 2021 and 2022, according to the Centers for Disease Control and Prevention (CDC). This accounts for roughly 1% of all adults in the U.S.
Epilepsy, also known as a seizure disorder, has no identifiable cause in about half of patients with the condition. Among the other half, it can be traced to a variety of factors, including genetic influence, head trauma, infections, injury before birth, and developmental conditions.
Depending on the type of seizure, symptoms can vary and affect any brain process. Those experiencing a seizure may suffer temporary confusion, loss of consciousness, a staring spell, stiff muscles, psychological symptoms like fear or anxiety, and uncontrollable jerking of the arms and legs.
But while anti-seizure medicine is a common treatment for most people who struggle with the disease, between 30% and 40% of patients have drug-resistant epilepsy. These patients do not respond to standard anti-seizure drugs.
Now, a new study conducted by researchers at UTHealth Houston has the potential to pave the way for personalized epilepsy treatments.
The team identified two genes tied to variants associated with epilepsy, revealing distinct traits that could make them valuable for diagnosing the condition.
This breakthrough links epilepsy to particular genetic mutations, offering a new perspective on the disorder and opening up possibilities for therapies that directly address its genetic roots.
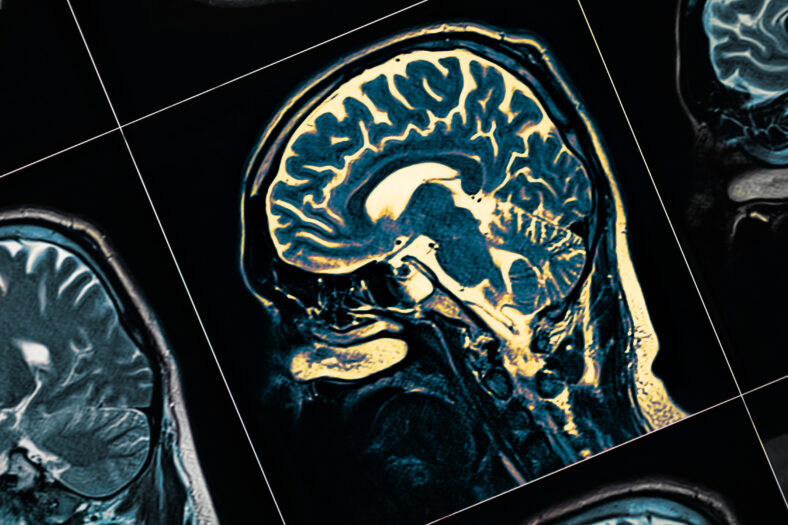
Under the leadership of Dennis Lal, the research team examined data from 1,386 human brain tissue samples of patients undergoing epilepsy surgery.
They focused on identifying somatic variants, or genetic changes that occur after conception and can only be detected in brain tissue itself.
Sign up for Chip Chick’s newsletter and get stories like this delivered to your inbox.
This study, the largest of its kind, led to the discovery of two new genes, DYRK1A and EGFR, along with the genetic mutations associated with brain lesions in epilepsy.
“Discovering these genes not only helps us better understand the biology behind epilepsy but also reveals specific traits in tissues, making them valuable tools for diagnosing the condition,” Lal explained.
The researchers were able to validate four known gene-disease links and provided evidence for eight additional ones.
Lal detailed how, once brain tissue testing following surgery becomes widely available in clinical settings, these results could finally shed light on the causes of drug-resistant epilepsy in patients.
Furthermore, the study found that several genes associated with epilepsy are involved in biological pathways that are targeted by cancer drugs approved by the FDA.
Although epileptic lesions and tumors share some genetic features, there are key differences. For instance, neurons affected by epilepsy do not multiply like cancer cells, suggesting that some cancer drugs could be repurposed for treating epilepsy.
“For those with epilepsy, their caregivers, and health care providers, our research represents a step closer to understanding epilepsy at its most fundamental level while improving patients’ quality of life,” Lal concluded.
To read the study’s complete findings, which have since been published in Nature Communications, visit the link here.
More About:News





